I want to start off by being completely honest and making the statement that you might not ever eliminate the antibodies to your thyroid gland one hundred percent. However, you can DRASTICALLY decrease them and have a much better functioning thyroid. As a result, your symptoms will decrease, your entire body will function better and you will feel a lot better. So, let’s start with a little overview.
The thyroid gland is a small butterfly-shaped gland in the throat, right below where the Adam’s apple is located in a man. Chronic Lymphocytic Thyroiditis, or Hashimoto’s disease, is an autoimmune disease where the immune system makes antibodies to the thyroid gland that damage the thyroid cells.
Antibodies are Y-shaped proteins that normally work to fend off disease-causing agents such as bacteria and viruses and keep us healthy. But in some people, the immune system can go haywire and the antibodies start attacking the body’s own tissues (like the thyroid gland in Hashimoto’s); hence, referred to as “auto-antibodies.” This damage interferes with the thyroid’s ability to make thyroid hormones.
An underactive thyroid, known as hypothyroidism, produces thyroid hormone levels that are too low and causes every function of the body to slow down. This is because the thyroid acts as the body’s metabolic control and thermostat. Brain function, heart rate, body temperature, and overall metabolic rate are all affected. Hashimoto’s is the most common cause of hypothyroidism and is 8 times more common in women than men, though I think that men are starting to play catch-up, based on observation alone.
What Causes Hashimoto’s
The body is complex and can react similarly to many different stressors. I like to say your body is like a drinking glass and stress from all facets of life is the water. For a while, you can pour in stress and your body will just hold it all in perfectly fine. Eventually, when you have poured just a bit too much from poor food choices, mental stress, environmental toxins, prescription or recreational drugs and alcohol or other forms of stressors, the body won’t be able to handle all of it and will overflow in the form of symptoms.
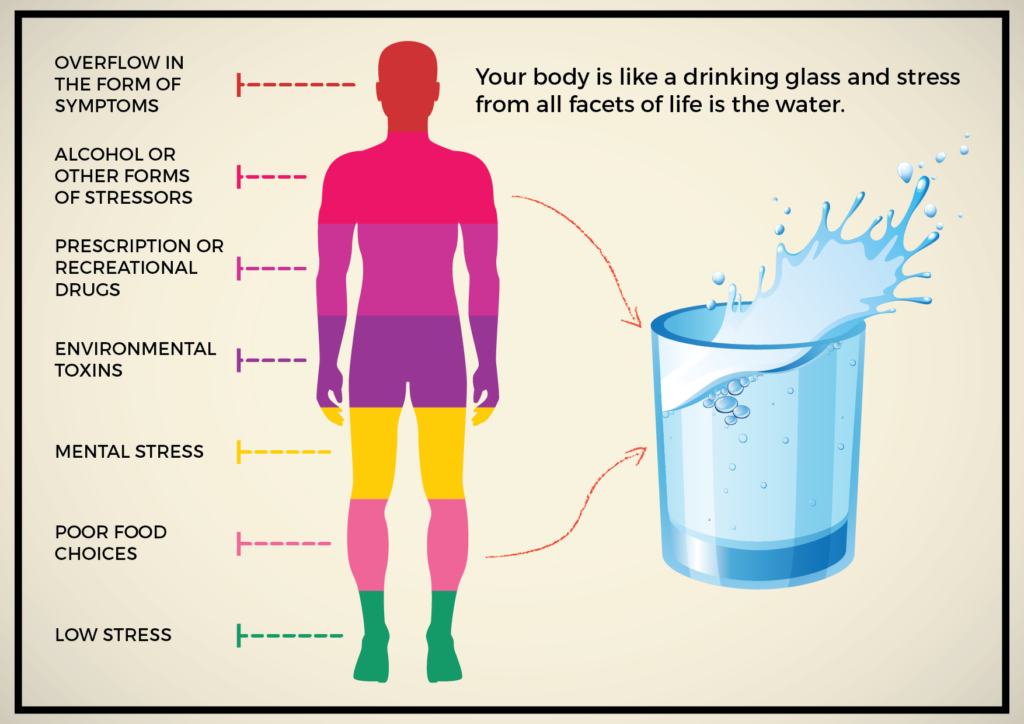
Your job is to notice these symptoms and fix the problem, not throw a towel under the glass and pretend it’s not overflowing anymore, which is often the same thing as taking prescription medications. Actually, your job should be to not allow the glass to get anywhere near full! However, pizza and beer are delicious, and I can sympathize with you!
Here are some commonly believed causes of Hashimoto’s.
- Genetic predisposition
- Viral or bacterial infection (Epstein Barr Virus, H. pylori)
- Parasitic infections
- Low good bacteria/high bad bacteria in the intestine
- Other autoimmune diseases, particularly Celiac disease: Hashimoto’s and Celiac disease may often coexist(1)
- Emotional/physical stress
- Pregnancy or recent childbirth
- “Leaky Gut Syndrome”
- Food allergies
- Gluten consumption
- Heavy metal toxicity/solvent exposure/others
- Deficient or ‘sub-optimal’ vitamin D levels
- Excess Iodine
- Unknown triggers for auto-antibody destruction
How to Know if you Have Hashimoto’s
Many people can have Hashimoto’s and have no symptoms for years. An enlarged thyroid is commonly the very first sign of the disease. If left untreated, symptoms tend to worsen over time.
These symptoms can include:
- Fatigue
- Decreased sex drive
- Weight gain
- Headache
- Pale, puffy face
- Difficulty swallowing
- Hoarse voice
- Cold intolerance (extreme sensitivity to cold)
- Joint and muscle pain
- Constipation
- Hair loss
- Thinning of eyebrows
- Heavy menstrual bleeding or irregular periods
- Psychological problems such as depression
- Mental slowness and memory issues
- Slow heartbeat
- Infertility
- High cholesterol
What are the Tests for Hashimoto’s?
Hashimoto’s is typically diagnosed through antibody testing in the blood, which includes Anti-thyroid peroxidase and Anti-thyroglobulin antibodies. It is quite common for Hashimoto’s to be associated with other autoimmune disorders such as Addison’s disease, type I diabetes mellitus, Grave’s disease, multiple sclerosis, pernicious anemia, celiac disease and more. When suspected of having Hashimoto’s disease, your doctor might order the following lab tests to confirm the diagnosis:
The following lab tests measure the health and production of the thyroid. These are typical results you might see if you have Hashimoto’s thyroiditis:
- Thyroid Stimulating Hormone (TSH): Elevated
- Free T4 (FT4): Low
- Free T3 (FT3): Normal to Low
- Reverse T3 (rT3): Normal to Elevated
The following two lab tests are the actual antibody tests for confirming the diagnosis of Hashimoto’s.
- Microsomal TPO-Ab: Elevated
- Thyroglobulin Antibodies: Elevated
The following lab test is the standard test for vitamin D levels and is low in the majority of Americans:
- Vitamin D, 25- Hydroxy: Low
- Ultrasound: “Ultrasound shows bi-lobar enlarged thyroid with the right lobe measuring at 7.4 cm x 2.3 cm and left lobe at 7.2 cm x 2.4 cm. No nodules seen in the thyroid.”
Basically this means the thyroid will be enlarged, due to a damaged thyroid having to work harder to try to keep up with thyroid hormone production. Nodules, or small masses in the thyroid, can sometimes occur and will have to be monitored by your physician.
Adrenal Stress Index– This test measures the cortisol levels in the saliva, taken at least four times a day for a clear picture of your cortisol levels and the condition of your adrenal glands. A commonly seen lab result in Hashimoto’s is low cortisol in the morning and low to normal cortisol throughout the day:

Total Salivary SIgA (Secretory Immunoglobulin A)– SIgA can be measured by testing the saliva or stool. This secretory version is different than IgA. So, don’t get the two tests confused. SIgA is produced anywhere in the body where there is mucus and is part of the first-line defense of the body. It protects us from foreign invaders, food particles and is related to food allergies and autoimmunity developing from poor gut health. It also keeps our healthy gut bacteria healthy!
Secretory IgA can be suppressed by disturbances in the GI tract or even hormones that are out of balance, related to the health of the hypothalamic-pituitary-adrenal (HPA) axis, mentioned again later in the adrenal gland section. What is an HPA axis? Just know that the hypothalamus and pituitary (located in the brain) are the master controllers of all other hormone-producing glands in the body and that all hormones can affect each other. So, it is important to keep the thyroid and adrenal glands well cared for.
This is what a SIgA test result can look like:
Low: <75.0 μg/ml—-> A Hashimoto’s patient is often in this range!
Equivocal: 75.0-145.0 μg/ml
High: 145.0-330.0 μg/ml
Food Allergies– Food allergies are commonly found in Hashimoto’s. Any of the IgE tests such as skin scratch/prick tests or blood IgE tests will likely show some positive food allergies, though these are somewhat unreliable. I will mention food allergies, testing and gut health more in the treatment section.
Heavy Metal Testing: This often shows high levels of cadmium, mercury and/or lead as observed by clinical experience.
Treatment for your Hashi’s (finally!)
I am going to assume for the purpose of this article that if you know you have Hashimoto’s Disease, your doctor has already run at least some of the appropriate labs and/or ultrasounds. If not, do those things first to evaluate where you stand. If you have thyroid nodules, that is beyond the scope of this article and needs to be discussed with your physician before moving on to treatment. A small percentage of nodules can become cancerous, which is something that requires further assessment and monitoring.
Thyroid Hormones
Depending on the severity of your symptoms and/or labs, your doctor can prescribe you the thyroid hormones levothyroxine (synthetic T4) and/or liothyronine (synthetic T3) or one of the porcine-derived thyroid prescriptions such as WP Thyroid, which naturally includes T4, T3 and trace amounts of thyroid cofactors (T1, T2, calcitonin and iodine).
There are benefits and drawbacks of each prescription option, with levothyroxine and liothyronine being synthetic but bioidentical whereas WP Thyroid is natural but non-bioidentical. Despite the route you and your doctor decide to take, they will increase your T4 and T3 and thus decrease your TSH levels.
When the master gland in the brain, (hypothalamus) senses that thyroid hormone levels are sufficient, it decreases the thyrotropin-releasing hormone (TRH), which in turn, normalizes the TSH production from the pituitary gland.. All these events occur because of the multi-feedback-loop, which connects the hypothalamus, pituitary, and thyroid with one another. Remember the HPA I mentioned earlier and how I said all of the hormone-producing glands were closely interconnected? Yeah…that!
Having a proper dose of thyroid hormones will give your thyroid a chance to rest and recuperate while you supplement with supporting herbs and nutrition, healing your body and building your thyroid function back up. This approach may also help you cut your future need of medications. Don’t worry, supplementing with thyroid hormone won’t negatively affect your thyroid’s natural ability to produce thyroid hormones in the future. Pregnancy can have an impact on your required dosage. So, tell your physician if you have a bun in the oven!
Supplements
There are fantastic supplements that directly support thyroid health and will help to heal your thyroid, quell your overactive immune system, and even help you eliminate the prescription thyroid hormones, if you’re taking them. They have a long history of safe and effective use. I am providing you with the exact supplements that many naturopathic, integrative and holistic physicians utilize to treat these conditions.
Blends of Direct Supporting Herbs/Nutrients
- Pure Encapsulations- Thyroid Support Complex: This formula contains selenium, which has been shown in studies to decrease thyroid antibodies. It also contains iodine and tyrosine to support thyroid hormone production. It includes a small amount of vitamin D and a good blend of supporting herbs.
Herbal Support
The next two are blends of herbs without the supporting vitamins and minerals. The previous supplement is best if you can only afford one. If you can afford more, I would personally also add in one of the following two or rotate them:
- Wise Woman Herbals- Thyroid I:
- Gaia Herbs- Thyroid Support Formula Pro:
Iodine
Iodine is required for your body to make thyroid hormones, among other things. However, there is conflicting data as to whether or not Hashimoto’s patients should take iodine. Most published research (2) shows that increasing iodine alone will dramatically increase the likelihood of developing antibodies to the thyroid gland and increasing thyroid cancer rates. This is especially displayed in people who started with low levels of iodine intake and then went to above-recommended levels (3).
This can be illustrated by the mostly worldwide addition of iodine to salt. While it eliminated the incidence of goiters and cretinism, especially in some third world countries, it also increased the rate of autoimmune thyroiditis, particularly in areas that have high iodine in their local food choices or are plagued with iodine contaminated water.(4)
In addition, supplements can be a source of excess iodine. A test performed and published in the New England Journal of Medicine 4 showed that among 25 randomly selected prenatal multivitamins containing iodine sources from kelp, 13 of them contained iodine levels that were different than their label stated by 50% or more, with the highest amount being 610 micrograms, or 170% more than the label stated and well above the WHO recommended daily intake for pregnancy. None of those were professional brands (professional brands tend not to use unreliable kelp as the iodine source or test each batch), and this is why it is important to purchase well-trusted professional sources of supplements.
I could spend a year and hundreds of pages writing about this topic alone. Since excess iodine has shown repeatedly to increase thyroid autoimmunity, I personally adhere to a conservative approach of consuming approximately the USDA’s Recommended Daily Intake of 150 micrograms for adults and 250 micrograms per day for pregnant or lactating women, as stated by the World Health Organization (5). This is from all sources- food, supplements, water, prescription drugs, etc. So, count your iodine intake well!
Here are a couple of supplements with doses in the microgram range, in case you decide you need it separately:
- Pure Encapsulations- Iodine and Tyrosine
- Progressive Labs- Iodine Capsules
Selenium
Selenium is a mineral that is required for thyroid hormone production. Not surprisingly, in humans it is found in the greatest concentration in the thyroid. It is also essential for the enzyme glutathione peroxidase (6) (GPx) to function. This enzyme assists the reduction of free radicals (in particular, hydrogen peroxide) by glutathione. So, the lack of selenium will impair the function of GPx, causing hydrogen peroxide to transform into even more dangerous free radicals and damage many parts of cells. The result is enhanced autoimmune destruction. Not good!
As the authors of this paper (7) stated, selenium intake is very important in the health of the thyroid and prevention of thyroid antibodies:
“The conclusion of our study is that even in mild selenium deficiency the supplementation of this important trace element has a significant impact on inflammatory activity in thyroid-specific autoimmune disease.”
The U.S. recommended daily allowance (8) for selenium is 55 micrograms, with thyroid patients typically being prescribed 200-400 micrograms (as supported by research), from both food and supplement sources, daily.
Here are two good sources of selenomethionine (the more absorbable form of selenium) supplementation in the typically recommended dosages:
- Now- Selenium 200 micrograms
- Pure Encapsulations- Selenium 200 micrograms
Tyrosine
Tyrosine is a non-essential amino acid that can be manufactured in the human body from the essential amino acid phenylalanine. Tyrosine is a precursor, or ingredient, to making thyroxine (T4), dopamine, epinephrine, norepinephrine and melanin. (9,10)
It is not often taken as a supplement since it is found in high amounts in commonly eaten food. Some fish, turkey, peanuts, beans and beef all have high levels of tyrosine. (11)
As stated above, it is well known that tyrosine is not only an ingredient to thyroid hormones but also to the stress hormones, norepinephrine and epinephrine. Some studies have shown that the body can direct tyrosine to the development of the chemical needed most. In other words, if a person is highly stressed, the body will direct the tyrosine to be used to manufacture the stress hormones instead of the thyroid hormones. (12, 13)
In rat studies, high stress leads to a lack of tyrosine for the thyroid and thus to lower levels of thyroid hormones. In humans, the hypothesis is that excess prolonged stress could lead to hypothyroidism in this same manner. Research has shown in humans that supplementing with tyrosine can improve the response to all sorts of stress-induced situations, both mentally and physically. (14)
I think the takeaway here is that excess prolonged stress should be avoided at all costs. We know it has many detrimental effects on the body and there is evidence that it can atleast decrease thyroid hormone levels acutely.
I don’t think supplementation with tyrosine is necessary unless you are under undue stress, which many of you might be from work overload, financial worries, relationship issues, etc. However, there is no evidence that tyrosine aids in the reduction of thyroid antibodies, which is the defining characteristic of Hashimoto’s.
If you think you might need a tyrosine supplement, here is a quality one:
- Genestra- Tyrosine 475mg Capsules
Indirect Strategies to Help the Thyroid
Heal the Gut:
The gut is the primary entryway into the body, delivering to us every molecule of food that we will ever ingest. It has a very specialized structure consisting of unique cells, glands, secretions, antibodies and connections between cells (called tight junctions) preventing allergens, beneficial organisms, harmful organisms, toxins and more from entering our bloodstream and causing harm to the actual “inside” of us while simultaneously allowing the good stuff in.
On top of that, there is a very complex and large orchestrated communication between the microbes, the immune system in the gut, the endocrine system in the gut and all the cells and proteins. In fact, there are oftentimes even more hormones and neurotransmitters that are produced here than in the brain! (15)
For these reasons, I believe that a healthy body starts with a healthy digestive system. So, it is a great place to start the repairs if you want to try to heal your Hashimoto’s.
To illustrate the importance of gut health, I like to use the analogy that the intestinal ecosystem is like Disney World on a Summer day. You have the parking lot and entry/ticketing area where there are thousands of people waiting and trying to get in and then you have the theme park area where there are workers and amusement rides that are all worthless unless people from the outside come to the inside and ride them and have fun. The two sides are separated by security cameras, fencing, gates, employees and security guards.
In this comparison, all of the food, bacteria, viruses and other microbes that we put into our bodies all day every day are the people trying to get into Disney World. The food will go inside and power all of the enzymes, cells and organs of the body. However, we too need fences and ropes and security guards to make sure no bugs get inside the park. Disney doesn’t want gang members inside their park causing trouble and destroying things and the body doesn’t want bugs inside of it doing the same thing. So we have immune cells, mucus, tight junctions, proteins, etc. that all patrol the gut and maintain a regulated barrier to entry.
Can you imagine if Disney removed all of their barriers to entry and just allowed anyone and everyone to come in at their own leisure? The park wouldn’t last a day, and neither would your body. That’s the extreme example. However, imagine if Disney decided to just remove one form of security or barriers? What if they left just one of the ten ticketing counters unsupervised or just removed the security guards? Would you feel safe? Would all sorts of people try to walk through the entry with no one there and would all sorts of people try to cause trouble with no security guards there? Of course. The park would go from a near-perfectly maintained and safe place to spend time with your children to a place where there are mostly good people but lots of bad guys getting in causing trouble too.
That is exactly how it is with your gastrointestinal system. If you skew the balance of good bacteria (security guards) with antibiotics, poor food choices, alcohol, etc., then the bad guys start taking over. Then, maybe you took too many painkillers that one time you injured your shoulder during that ski trip and damaged some of the lining of your gut or perhaps you have a genetic predisposition to gluten intolerance and you had too much wheat this year and now the glue between the intestinal cells has weakened and the gates are down allowing thugs into the body?
Every little bit of damage adds up over the years, and eventually, the balance gets tilted to where symptoms start to occur and disease begins to manifest. Again, we have to maintain a healthy gut to be healthy and we have to heal the gut to heal the body.
In the causes section, I mentioned food allergies, good and bad bacteria, parasites and “leaky gut” as being possible reasons for developing Hashimoto’s. In reality, these are mostly one in the same, because if one goes awry, they (eventually) all go awry. It all goes back to the health of the bacteria and yeast populations and the intestinal wall. Many research studies have revealed a link (16) between autoimmune diseases and both damage to the intestinal lining and an unhealthy bacteria populations. (17)
You might have heard of the term “leaky gut” over the last few years, as it has been gaining in popularity. Look at how many research papers have been published in recent years on “autoimmune and gut”!

A leaky gut is a danger signal for autoimmune diseases (18), including Hashimoto’s. It’s basically where damage to the intestinal lining (19) allows incompletely digested food (especially proteins) to flow through into the bloodstream where they’re able to provoke an autoimmune response. This is called increased intestinal permeability. It starts the chain reaction that, it’s believed, leads to your immune system attacking itself and causing auto-immune disease. Supplementing the thyroid is great, and can help a ton with function, but if you want to truly fix the problem, you have to fix the underlying cause. Heal the gut!
The first step to healing the gut is to remove anything you’re ingesting that is causing damage to your GI tract. This includes junk food, gluten (20), alcohol (yes, I know…sorry), antibiotics (you can’t start fixing your gut until these are finished), some over-the-counter drugs such as Ibuprofen and any foods you have allergies to. This will decrease the intestinal permeability and inflammation in the GI tract, allow healthy bacteria to flourish again with supplementation, decrease the immune response in the body and allow you to heal faster.
There are many tests to determine if you have food allergies, but most are fairly unreliable or irrelevant. I won’t get into food allergy testing here but the best method to determine what foods you are allergic to, especially when you have a more severe case of food allergies, is what I call the “from scratch” method.
This is where you eliminate everything from your diet and start over with only a handful of foods you’ve never eaten before all while supplementing appropriately and allowing your gut to heal. Then, you gradually add one food type back into your diet every few days and watch for any reactions. The simplest way to do this is to make a food diary and note every thing you put in your mouth and any accompanying reactions you may experience so you can easily track what food triggered the disturbance. Add any problematic foods to your “do not eat” list.
Of course, a much simpler method for milder cases is simply eliminating the most common suspects and observing if that eliminates your symptoms. In many people it does.
According to the American Academy of Allergy, Asthma & Immunology (AAAAI) (21), and Kamer and fellow researchers (22), the following eight foods are responsible for about 80% of IgE mediated allergic reactions (the type of antibody that causes immediate symptoms, like a bee sting. There are also non-IgE mediated food allergies.
- Cow’s milk
- Eggs
- Fish
- Peanuts
- Shellfish
- Soy
- Tree nuts
- Wheat
Now that you’ve lowered the immune response by eliminating food allergies, you can begin to minimize inflammation, replace the beneficial bacteria and yeasts and heal the intestinal lining. Here are some supplements that are highly used and recommended by doctors:
Demulcents
These act to coat and soothe the GI lining. It’s like a protecting ointment for the intestinal tract. Since the mucous layer is often depleted, these will help! Choose one from this group:
- Bioclinic Naturals- Deglycyrrhizinated Licorice (DGL): Light Licorice Flavor – Chew a couple before each meal!
- Nature’s Way- Marshmallow herb: liquid or capsules
- Pure Encapsulations- DGL Plus– Combination demulcent (soothing) product in capsule form
Blended Products
- Innate Response- GI Response Powder
- Pure Encapsulations GI Fortify powder and capsules
Probiotics
I think we’ve mentioned the importance of a healthy bacteria colony in the gut plenty already! Just remember to purchase a quality brand with a good reputation. You want a product with atleast 1 billion CFU (colony forming units) per dose, because they won’t all survive the trip to the intestines. You also want a product rich in Lactobacillus and Bifidobacterium, because research shows that those two types are the most abundant and do the most good.
Importantly, don’t forget the yeast! Not all yeast is bad, just like not all bacteria is bad. Saccharomyces boulardii is a species of the yeast that has been used as a probiotic for decades. Studies (23) prove that this yeast strain can fight Clostridium infections, raise secretory IgA levels and increase the mucus barrier in the gut. Not bad for one little bug.
One more thing, if you’re purchasing probiotics online, pay for the overnight delivery if it’s hot outside. Probiotic supplements can be exposed to high temperatures for brief periods of time but you don’t want a 6-day transit in the Summer season.
- Seroyal HMF Forte Probiotic
- Klaire Labs- Saccharomyces boulardii yeast
- Fermented Foods- Don’t forget that huge amounts of live bacteria can be found in some delicious foods right at your local grocery store. They have to be naturally fermented foods, not pickled with vinegar. Foods like naturally fermented sauerkraut, kimchi and organic natto (watch for soy allergies on this last one) are amazing ways to restore your gut bacteria. Try eating a few servings a day during the healing process. I like to switch brands (or ferment my own foods) and get varied strains of bugs. My kids even eat sauerkraut like salsa with organic corn chips and on their grass-fed hot dogs!
Fish Oil
The omega 3 fats, including EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid), possess strong anti-inflammatory properties. Because inflammation is a feature of autoimmune diseases (24), including Hashimoto’s, maintaining an adequate intake of omega 3 fats is of utmost importance to limit thyroid inflammation and damage. For people suffering from inflammatory disease states, such as autoimmune diseases, cancer, arthritis or high cholesterol, 2-3 grams per day of omega 3 fatty acids are probably required to decrease inflammatory markers in the body and have any useful effect (25). The USDA recognizes up to 3 grams per day as safe and the European Union recognizes up to 5 grams per day (26) as safe. I’ve even heard of people going much higher with no reported negative side effects.
Even though high-quality fish oil supplements have been proven to be safe for patients with fish allergies (27), I would always recommend testing a small amount before going into full doses.
Adrenal Support
The thyroid gland is intimately related to the hypothalamic-pituitary-adrenal (HPA) axis. The hormonal system is like an intricate web where all parts are connected. If something goes wrong with one of them, it very often disrupts the others.
Elevated TSH is associated with elevated cortisol, but the opposite is also very well-known to be true. To normalize your thyroid levels and immune function, the appropriate amount of cortisol is necessary, which is why these selected supplements contain a lot of adaptogenic (adapting) herbs, good for both your thyroid and adrenal glands (28,29).
- Pure Encapsulations: Phyto ADR This contains 150 mg of vitamin B5 and Panax ginseng extract (root), 100 mg of Eleutherococcus senticosus extract (root), 150 mg of a popular and highly beneficial adaptogen called ashwagandha extract (root), and 50 mg of Rhodiola rosea extract (root).
Vitamin D
Extensive research (30) reveals that low levels of vitamin D play a role in autoimmune diseases (31), including Hashimoto’s. This sunshine vitamin has a potential to suppress an overactive immune system, thus, benefiting people with Hashimoto’s. Part of that reason is because vitamin D promotes healthy T and B cell function (32). These cells can become autoreactive, leading to the production of antibodies that attack their own body. Ensuring adequate vitamin D intake is essential if you have an autoimmune condition.
In addition to increasing your exposure to natural sunlight, several foods such as wild Alaskan salmon can supply sufficient amounts of vitamin D. The vitamin D recommendations provided by various American health organizations (33) are as follows:
- Vitamin D Council: About 5,000 IU (international units) of vitamin D daily with the maximum recommended dose being 10,000 IU per day.
- Endocrine Society: Around 1,500 – 2,000 IU per day with the maximum recommended dose being 10,000 IU daily.
- Food and Nutrition Board: 600 IU of vitamin D daily for adults below the age of 65 years and 800 IU per day for seniors but no more than 4,000 IU daily.
Here are a few very high-quality sources of vitamin D supplementation:
- Genestra- D-Mulsion Liquid 1,000 IU
- Pure Encapsulations- Vegan Vitamin D Liquid 1,000IU
- Allergy Research Group- Vitamin D Complete
In addition, vitamin D can be obtained from dietary sources. Here are some of the best ones:

Of course, swordfish and tuna are very high in mercury and should only be eaten very rarely.
Don’t forget the good ol’ fashioned sun! Spending some time under the sun also helps get vitamin D. With that said, try to avoid sun exposure exceeding 20 to 25 minutes at one time. Other than getting the necessary amount of vitamin D, being outside will also help release feel-good brain chemicals to fight the blues of an underactive thyroid. Which leads me to…
Stress Management
Stress is a huge factor in disease in our modern life. We are under more stress today than we have ever been as a species. Sure, sometimes a lion came and ate a family member or the king’s guard came and burned down your house once in a while, but those were infrequent events. Now, many people are stressed from the moment they wake up until late at night when they finally fall asleep because stress is keeping them up at night. Think about it, getting kids ready for school, morning traffic, running late for work, not having time for breakfast, forgetting the proposal for the meeting at home, fear of being fired, fighting with your spouse, mortgage and other bills, etc. etc. Just reading that list is stressful and exhausting!
Let’s forget about the research studies for a minute here. Just think about how awful you feel when you’re stressed. You might binge eat or you might not eat at all, you can’t even get your thoughts together clearly when fighting with your spouse, you may get nervous, anxious, perhaps you experience heart palpitations, the list of physical side effects is very well known to all of us. If you don’t think stress also has a long-term effect on the health of the body, you are probably going to be the first of us to go!
So, let’s remember to reduce the stress in our lives because it makes a very strong impact on our lives, the lives of our loved ones and all of our health. Find time to do something you love to help calm your mind and let the stress dissipate. Exercising, journaling, yoga, meditating, painting, anything can work! Relaxation techniques like deep breathing also help reduce the stress response when you feel it overwhelming you. There are tons of apps and videos on these types of things, guided meditations, and much more readily available to anyone with a cell phone. Reducing your stress will help to normalize the function of the adrenal glands and thus the thyroid gland. Let’s all take a deep breath before we continue reading. 🙂
Infection
There have been some studies that have linked thyroid disease, cancer and some other illnesses to viruses such as the Epstein-Barr (34) (EBV) and to parasites such as Toxoplasma gondii (35,36) (causes toxoplasmosis). The research shows a high correlation, or relationship, but not yet that the virus or parasite is the cause of the thyroid disease. It could be very well that the infection causes thyroid disease or perhaps thyroid disease makes the body susceptible to infections. We do not yet know for sure.
Since we don’t yet have a good cure for viruses, the best thing you can do at this point is to stay as healthy as you can, keeping your immune system in shape to fight off infections as best it can. If you are concerned you may have a parasite infection, this can be tested by your physician with blood and/or stool samples.
Heavy Metals
I mentioned heavy metals in the testing section towards the beginning of this article. Unless you have a very high acute exposure, you probably won’t test for high levels of metals like lead in your blood. Because heavy metals are not very well eliminated, and they don’t float around in the blood much (they are often stored in organs and bones), most physicians specializing in environmental medicine will use what is called a “challenged elimination test”. This is where you are given a supplement that binds to metals in the body and allows the body to eliminate the metals. Often, this supplement, called a chelation agent, is in the form of a capsule and you will collect your urine for a specific time after taking the capsules and send to the lab for analysis. This method allows doctors to see how much heavy metal is bound by the supplement and eliminated from your body.
If your test results show that you do have high levels of heavy metals, a proper chelation protocol will be warranted to aid your body in eliminating those. Unfortunately, heavy metal toxicity can exhibit a huge variety of symptoms, including autoimmunity, as some studies (37) have shown.
In addition, industrial chemicals and/or pesticides such as polyaromatic hydrocarbons (38,39) (gasoline, burning wood, burning coal), polybrominated biphenols (40) (flame retardants, plastics), and polychlorinated biphenols (41) (plastics, dyes, construction materials) have been shown to induce thyroid disease (42). These chemicals are abundant in our modern environment and every single one of us is exposed to them on some level. There are also tests for these types of chemicals. It is very important to avoid these types of chemicals as best you can and get tested if you think you may have had any sort of exposure.
What are the Food Guidelines for Autoimmune Thyroid Disease?
1) Cut back on foods that may trigger or worsen your immune system.
These foods may promote inflammation in those with an overactive immune system. Every individual reacts differently to different foods. So, the best strategy is to use the from-scratch method, mentioned previously.
Dairy
A person with an autoimmune disease like Hashimoto’s must avoid dairy like the plague! Dairy is considered one of the biggest villains for autoimmune disease sufferers. As mentioned previously, it is the most common foods to have a food allergy to.
There’s an exhaustive list of dairy products that need to be avoided, at least in the initial elimination phases and until you have determined what foods you’re allergic to. However, I personally try to never eat dairy foods. They have too many downsides and there are so many good substitutes these days. Have you tried the new Ben & Jerry’s non-dairy ice cream flavors? They are amazing but watch out for other ingredients that are not on your diet!:
- Milk (including condensed, dry, evaporated, goat or cow’s milk, low-fat, nonfat, powder, protein, skimmed)
- Butter
- Buttermilk
- Cheese (all types, including cottage cheese)
- Cream, including sour cream and sour cream solids
- Yogurt
- Ice creams
- Custard/pudding/trifle
- Casein (sometimes used as a protein supplement)
- All kinds of caseinates
- Whey protein (the major whey allergens are Lactalbumin, Lactoglobulin, and Lactoferrin)
- Ghee (aka clarified butter; pure ghee contains 90-95% of butter oil)
- Half-and-half – a beverage that contains equal amounts of whole milk and light cream
- Milk and coffee drinks (aka Latte)
Beware of the products labeled as “non-dairy” (43) that may contain hidden milk substitutes. Such products include:
- Baked goods
- Cakes, cookies, and pastries brushed with milk
- Chocolate or other candies made with milk or cream
- Margarine (may contain trace amounts of dairy)
- Salad dressings like ranch or side dip; some mayos contain cream
- Some meats may include casein as a binder; others like steaks may have been drizzled with butter for enhancing the flavor
- Fish dipped in milk to minimize the fishy odor
- Individuals who are allergic to cow’s milk are often advised to also avoid milk from other animals as well
Grains
There are several types of grains that can be especially problematic for people with autoimmune diseases. These include the gluten-containing grains that have the potential to increase intestinal permeability and set off an immune response, wreaking havoc on your immune system, as occurs in Celiac disease. Wheat, rye and barley all belong to this category.
Gluten is a general name for one of the proteins found in wheat (durum, emmer, spelt, farina, farro, KAMUT® khorasan wheat and einkorn), rye, barley and triticale. Gluten helps food maintain its shape, acting as a glue that holds it together. Gluten can be found in many types of foods, even ones that would not be expected. So, read your labels carefully!
It is often discussed if oats have gluten in them and if they are okay to eat for people avoiding gluten. The terminology gets a little complex here but essentially gluten is a mixture of proteins. Wheat gluten contains a smaller protein called gliadin, which is the actual part that celiac patients react to. In barley, the smaller protein is called hordein; in rye, it is named secalin and in oats it is known as avenin (44, 45). Some people with Celiac disease will react to the avenin in oats (46) and some will not, at least not on a noticeable level. So, this food should also be removed, or at least tested by removing it from the diet and re-testing it down the road. Lastly, oats are commonly contaminated with wheat products. So, make sure yours are certified “gluten-free.”
Here are some common foods that contain gluten:
- Pasta:
- ravioli, dumplings, couscous, and gnocchi
- Noodles:
- ramen, udon, soba (those made with only a percentage of buckwheat flour), and egg noodles. (Note: rice noodles and mung bean noodles are gluten free)
- Bread and Pastries:
- croissants, pita, naan, bagels, flatbreads, cornbread, potato bread, muffins, donuts, rolls
- Crackers:
- pretzels, goldfish, graham crackers
- Baked Goods:
- cakes, cookies, pie crusts, brownies
- Cereal & Granola:
- corn flakes and rice puffs often contain malt extract/flavoring, granola often made with regular oats, not gluten-free oats
- Breakfast Foods:
- pancakes, waffles, french toast, crepes, and biscuits.
- Breading & Coating Mixes:
- Breadcrumbs, panko breadcrumbs
- Croutons:
- stuffings, dressings
- Sauces & Gravies (many use wheat flour as a thickener)
- traditional soy sauce (though tamari is made without wheat and is gluten-free), cream sauces made with a roux
- Beer (unless explicitly gluten-free) and any malt beverages
- Brewer’s Yeast
- Energy bars/granola bars – some bars may contain wheat as an ingredient, and most use oats that are not gluten-free
- French fries – be careful of batter containing wheat flour or cross-contamination from fryers
- Potato chips – some potato chip seasonings may contain malt vinegar or wheat starch
- Processed lunch meats
- Candy and candy bars
- Soup – pay special attention to cream-based soups, which have flour as a thickener. Many soups also contain barley
- Multi-grain or “artisan” tortilla chips or tortillas that are not entirely corn-based may contain a wheat-based ingredient
- Salad dressings and marinades – may contain malt vinegar, soy sauce, flour
- Starch or dextrin if found on a meat or poultry product could be from any grain, including wheat
- Brown rice syrup – may be made with barley enzymes
- Meat substitutes made with seitan (wheat gluten) such as vegetarian burgers, vegetarian sausage, imitation bacon, imitation seafood (Note: tofu is gluten-free, but be cautious of soy sauce marinades and cross-contamination when eating out, especially when the tofu is fried)
- Pre-seasoned meats
- Anything else that uses “wheat flour” as an ingredient
Oils and Fats
Vegetable oils such as corn, cottonseed, sunflower and safflower oil have high levels of omega 6 fatty acids and little-to-no omega 3 fatty acids. It is recommended that we consume a ratio somewhere between 1:1 to 1:4 omega 3 fatty acids to omega 6 fatty acids (47). Unfortunately, in western society we tend to consume about a 15:1 ratio.
Omega 6 oils do more harm than good when consumed in excess. They are a precursor to inflammatory chemicals in the body (48), which are quite the opposite of the health-friendly and anti-inflammatory omega-3 fatty acids. High intake of omega 6 fatty acids are risky for someone with an autoimmune disease.
Try to stick with cold pressed oils that are higher in omega 3 fatty acids:
| Food | Grams Per Serving | ||
| ALA | DHA | EPA | |
| Flaxseed oil, 1 tbsp | 7.26g | ||
| Chia seeds, 1 ounce | 5.06g | ||
| Hemp Seed Oil, 1 tbsp | 3.1g | ||
| English walnuts, 1 ounce | 2.57g | ||
| Flaxseed, whole, 1 tbsp | 2.35g | ||
| Walnut Oil, 1 tbsp | 1.44g | ||
| Canola oil, 1 tbsp | 1.28g | ||
| Soybean oil, 1 tbsp | 0.92g | ||
| Black walnuts, 1 ounce | 0.76g | ||
| Edamame, frozen, prepared, ½ cup | 0.28g | ||
| Salmon, pink, canned, drained, 3 ounces* | 0.04g | 0.63g | 0.28g |
| Salmon, Atlantic, farmed cooked, 3 ounces | 1.24g | 0.59g | |
| Salmon, Atlantic, wild, cooked, 3 ounces | 1.22g | 0.35g | |
| Herring, Atlantic, cooked, 3 ounces* | 0.94g | 0.77g | |
| Sardines, canned in tomato sauce, drained, 3 ounces* | 0.74g | 0.45g | |
| Mackerel, Atlantic, cooked, 3 ounces* | 0.59g | 0.43g | |
| Trout, rainbow, wild, cooked, 3 ounces | 0.44g | 0.4g | |
| Sea bass, cooked, 3 ounces* | 0.47g | 0.18g |
Table sources- Ensminger AH, Konlande JE. In: Foods & nutrition encyclopedia. Ensminger AH, Konlande JE, editor. CRC Press; 1993. Fats and other lipids; p. 691. USDA National Nutrient Database for Standard Reference, Release 22. October 10 2009. http://www.nal.usda.gov/fnic/foodcomp/search/ February 18, 2010. Government of Canada Nutrient Profile. https://food-nutrition.canada.ca/cnf-fce/report-rapport.do
Because non-animal sources of omega 3 fatty acids don’t offer the components called EPA and DHA, the best food sources of omega 3 fatty acids are smaller cold-water fish such as wild caught salmon and sardines. The American Heart Association (49) recommends eating a serving of this type of fish at least two times per week.
It should also be noted that most meat naturally contains high ratios of omega 3 fatty acids when the animal is eating its natural diet, such as grass-fed and grass-finished steak or wild-caught fish. However, when a cow, for example, is switched to grain, the ratio and total amount of omega 3 fatty acids goes down (50,51) significantly.

Fruits and Vegetables
Fruits and vegetables provide a huge source of nutrients including: fiber, vitamins, minerals, carotenoids, polyphenols and more! An abundance of research reflects the importance a diet high in fruits and vegetables has on decreasing many diseases (52) and lowering overall mortality rates.
Polyphenols are a family of versatile plant-based chemicals that are present in colorful fruits and vegetables. There have been over 8,000 polyphenols discovered so far (53) with over 4,000 of them being flavonoids!
Polyphenols are well-known for their potent antioxidant activities. They can stimulate the formation of glutathione (54) by enhancing enzyme activity, which protects against free radical injury and the development of auto-antibodies.
Some of the best sources of polyphenols include:
- Berries
- Peaches
- Pears
- Pomegranates
- Green tea
- Spinach
- Broccoli
- Cabbage
Directly related to Hashimoto’s Thyroiditis, some of these healthy foods contain high levels of sulfur, which is a mineral required by your body to perform various tasks, one of which is the formation of glutathione (55). It is found in two amino acids in our diet, namely cysteine and methionine. Hence, a diet rich in these amino acids will suffice your requirement of sulfur and subsequently raise GSH levels.
The dietary sources of sulfur include:
- Cruciferous veggies such as cauliflower, cabbage, broccoli, Brussel sprouts, bok choy, garden cress, kale, Collard greens, arugula, kohlrabi
- Poultry
- Fish
- Beef
Vitamin C and Vitamin E are potent antioxidants and are also found in fruits and vegetables. Vitamin C is a water-soluble vitamin that has the potential to raise the glutathione levels in the red and white blood cells (56). Vitamin E is fat-soluble and partners with vitamin C to remove the damaging free radicals (57). Vitamin C also helps to regenerate vitamin E, thus fighting the free radicals repeatedly.
Watch out for Nightshades!
These include potatoes, tomatoes, sweet and hot peppers, eggplant, tomatillos, pepinos, pimentos, paprika, cayenne pepper, belonging to the family, Solanaceae. While the nightshade foods do carry health benefits, they can also have a downside to some people. Research (58) shows that these plants contain chemicals that can be toxic to our bodies.
Avoiding/limiting the intake of nightshades can be an important part of a low inflammation diet (59). I would personally address this component of the diet last, as some research has shown that cooking reduces the toxic chemicals. In addition, they also can provide some beneficial aspects in proper doses such as regulation of heart beat rate and force of contractions (60).
HEAP ON THE NUTRIENTS THAT ARE BENEFICIAL FOR YOUR IMMUNE SYSTEM!
Glutathione Rich Diet
Composed of short chains of three amino acids, glutathione (GSH) is produced in almost every cell of your body. Is it a very important and powerful antioxidant and detoxifying agent in the body. How does this help someone with an autoimmune disease?
GSH serves to neutralize free radicals. Because free radicals cause oxidative damage, GSH is considered to be a potent “antioxidant.” Free radical-induced body damage plays a pivotal role in autoimmunity (61). Moreover, a variety of factors like poor diet, aging, and poor health can deplete the GSH stores over time leading to, or worsening, autoimmune damage. Supplementing glutathione in such cases then becomes essential. In fact, antioxidant therapy of autoimmunity (62) has been a subject of great interest.
Another predominant function of GSH is detoxification – i.e. helping your body get rid of the toxins. Research reveals that the body of people with autoimmune diseases may lack the capability to get rid of the toxins (63) on a daily basis. This leads to what is called “bioaccumulation”, toxins entering the body faster than the body can eliminate them causing havoc throughout the system. In contrast, adding GSH can benefit a great deal by detoxifying and rejuvenating your body.
There are a variety of foods that contain a good amount of GSH. Working the following foods into your diet can increase the glutathione levels in your body (64):
- Asparagus (contains about 28.3 mg of GSH)
- Avocado (contains about 27.7 mg of GSH)
- Raw spinach (contains about 12.2 mg of GSH)
- Okra (contains about 12.0 mg of GHS)
- Cauliflower (contains about 9.1 mg of GSH)
- Walnuts (contains about 15.1 mg of GSH)
Selenium Rich Diet
I mentioned selenium earlier in the supplement section. Just remember that if you aren’t supplementing with selenium, you need to make sure you are eating foods with good levels of it, as many sources state that our soils are commonly depleted of this required mineral and food sources are lower in selenium than they used to be.
Selenium-rich sources along with their percent of recommended daily allowance are as follows:

Information source: https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/#en10
GOITROGENS
I will make this section short and sweet. Disregard any information on goitrogens from food you’ve ever heard. There are zero human studies and no good animal studies showing any negative goitrogenic effects from food sources (one study even showed a decrease of thyroid cancer with high cassava consumption!).
Please eat as many vegetables of any type as you would like. The only goitrogens you should be concerned about are from prescription drugs and environmental toxins. Here are some of the main culprits: amiodarone (contains 37% iodine) and lithium (prescriptions), polyaromatic hydrocarbons (combustion engines), polybrominated biphenols, and polychlorinated biphenols (plastics, coolant, engine oil). (65)
General Hashimoto’s Diet Plan:
| Vegetables | All vegetables, especially leafy greens. Aim to eat vegetables from all the colors of the rainbow each day including: anise, artichoke, asparagus, beets, bok choy, broccoli, cabbage, carrots, cauliflower, celery, chives, cucumbers, garlic, kale, kohlrabi, leeks, lettuce, mustard greens, onions, parsley, radishes, rhubarb, shallots, spinach, squash, sweet potatoes, water chestnuts, watercress, yams, zucchini. |
| Fermented Foods | Fermented foods are beneficial to gut health and modulating the immune system. Sauerkraut, kimchi, pickled ginger, fermented cucumbers, coconut yogurt, kombucha, water kefir |
| Meats | Emphasize organic, grass-fed grass-finished beef and bison, organic pastured free-range chicken, lamb and turkey, seafood and wild-caught fish, pastured omega 3 eggs (if tolerated) |
| Low Glycemic Fruits | Apples, apricots, avocados, berries, cherries, grapefruit, lemons, oranges, peaches, pears, plums. |
| Nuts and Seeds | Walnuts, pecans, almonds, brazil nuts, pumpkin seeds, sunflower seeds, coconut, etc. Raw, roasted, or nut butters |
| Herbs and Spices | Basil, cilantro, coriander, cumin, garlic, ginger, lemongrass, mint, oregano, parsley, rosemary, sage, sea salt, thyme, turmeric, etc |
| Legumes | chickpeas, beans, lentils, etc. |
| Grains | Grains should be avoided until inflammation has decreased and immune response is under control. Gluten-free grains such as buckwheat, quinoa, rice and corn may be tolerated by some. |
| Others | Apple cider vinegar, herbal teas, olive oil, olives, avocado, coconut oil |
Ideas for food substitutions:
| Instead of This… | Use This…. |
| Refined Industrial Seed Oils like Canola, Soy, Corn, Safflower | Olive oil, avocado oil, macadamia oil, walnut oil, sesame oil |
| Breadcrumbs of flour | Almond flour, cashew flour, tapioca starch, arrowroot starch |
| Thickeners (wheat flour, cornstarch) | Tapioca starch, arrowroot starch, blended roasted vegetables |
| Pasta | Spaghetti squash, spiralized zucchini, beet, carrot, etc. |
| Rice | Cauliflower |
| Milk, cream or yogurt | Coconut milk, almond milk, hemp milk |
| Sugar | Xylitol, ripe bananas or dates |
| Soy sauce | Bragg’s Liquid Aminos, fish sauce |
| Tofu | Meat, fish, seafood, or extra vegetables |
| Peanut butter | Almond, cashew, pecan, hazelnut, or macadamia nut butter |
Overview:
- Eliminate potential causes of autoimmunity
- Viral/bacterial/parasitic infection (improve health of immune system)
- “Leaky Gut Syndrome” and dysbiosis (high bad bacteria, low good bacteria in gut)
- Other autoimmune diseases, particularly Celiac disease
- Emotional/physical stress
- Food allergies
- Heavy metal toxicity/solvent exposure
- Deficient or ‘suboptimal’ vitamin D levels
- Look into taking thyroid hormones to support the required levels in the body while healing the thyroid gland
- Take supplements to support the thyroid function and the HPA axis
- Maintain a healthy, low inflammatory diet to keep the intestinal tract in good function and the body with a steady supply of the nutrients, vitamins, minerals it needs to operate properly
Would you like a consultation regarding your Hashimoto’s? Please send me an email here with the title “Hashimoto’s”!
References
- Lerner, A., Jeremias, P., & Matthias, T. (2017). Gut-thyroid axis and celiac disease. Endocrine Connections, 6(4), R52-R58. doi:10.1530/ec-17-0021 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5435852/
- Ruben Harach, H., & Williams, E. (1995). Thyroid cancer and thyroiditis in the goitrous region of Salta, Argentina, before and after iodine prophylaxis. Clinical Endocrinology, 43(6), 701-706. doi:10.1111/j.1365-2265.1995.tb00538.x https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2265.1995.tb00538.x
- Weiping Teng, M.D., Zhongyan Shan, Ph.D., Xiaochun Teng, M.D., et al. (2006). Effect of Iodine Intake on Thyroid Diseases in China | NEJM. (2018). New England Journal of Medicine, 354:2783-2793. DOI: 10.1056/NEJMoa054022 https://www.nejm.org/doi/10.1056/NEJMoa054022?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200www.ncbi.nlm.nih.gov
- Luo, Y., Kawashima, A., Ishido, Y., Yoshihara, A., Oda, K., & Hiroi, N. et al. (2014). Iodine Excess as an Environmental Risk Factor for Autoimmune Thyroid Disease. International Journal Of Molecular Sciences, 15(7), 12895-12912. doi:10.3390/ijms150712895 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4139880/
- WHO | Iodine supplementation in pregnant and lactating women. (2018). Who.int. Retrieved 26 July 2018, from https://www.who.int/elena/titles/guidance_summaries/iodine_pregnancy/en/
- Lubos, E., Loscalzo, J., & Handy, D. (2011). Glutathione Peroxidase-1 in Health and Disease: From Molecular Mechanisms to Therapeutic Opportunities. Antioxidants & Redox Signaling, 15(7), 1957-1997. doi:10.1089/ars.2010.3586 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3159114/
- Gärtner, R., Gasnier, B., Dietrich, J., Krebs, B., & Angstwurm, M. (2002). Selenium Supplementation in Patients with Autoimmune Thyroiditis Decreases Thyroid Peroxidase Antibodies Concentrations. The Journal Of Clinical Endocrinology & Metabolism, 87(4), 1687-1691. doi:10.1210/jcem.87.4.8421https://academic.oup.com/jcem/article/87/4/1687/2374966
- Office of Dietary Supplements – Selenium. (2018). Ods.od.nih.gov. Retrieved 25 July 2018, from https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/
- “tyrosine.” The Columbia Electronic Encyclopedia. © 1994, 2000-2006 on Infoplease.
© 2000-2017 Sandbox Networks, Inc., publishing as Infoplease.
8 Aug. 2018
https://www.infoplease.com/encyclopedia/science/biochemistry/concepts/tyrosine - “phenylalanine.” The Columbia Electronic Encyclopedia. © 1994, 2000-2006 on Infoplease.
© 2000-2017 Sandbox Networks, Inc., publishing as Infoplease.
8 Aug. 2018
https://www.infoplease.com/encyclopedia/science/biochemistry/concepts/phenylalanine - Food Composition Databases Show Nutrients List. (2018). Ndb.nal.usda.gov. Retrieved 9 August 2018, from https://ndb.nal.usda.gov
- Khaliq, W., Andreis, D., Kleyman, A., Gräler, M., & Singer, M. (2015). Reductions in Tyrosine Levels are Associated with Thyroid Hormone and Catecholamine Disturbances in Sepsis. Intensive Care Medicine Experimental, 3(Suppl 1), A686. doi:10.1186/2197-425x-3-s1-a686 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4798095/
- Research, I., & Marriott, B. (1994). Tyrosine and Stress: Human and Animal Studies. National Academies Press (US). Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK209061/
- Rivlin, R., & Asper, S. (1966). Tyrosine and the thyroid hormones. The American Journal Of Medicine, 40(6), 823-827. doi:10.1016/0002-9343(66)90198-7 https://www.amjmed.com/article/0002-9343(66)90198-7/pdf
- Tan, D., Manchester, L., Terron, M., Flores, L., & Reiter, R. (2007). One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species?. Journal Of Pineal Research, 42(1), 28-42. doi:10.1111/j.1600-079x.2006.00407.x https://onlinelibrary.wiley.com/doi/full/10.1111/j.1600-079X.2006.00407.x
- Tlaskalová-Hogenová, H., Štěpánková, R., Kozáková, H., Hudcovic, T., Vannucci, L., & Tučková, L. et al. (2011). The role of gut microbiota (commensal bacteria) and the mucosal barrier in the pathogenesis of inflammatory and autoimmune diseases and cancer: contribution of germ-free and gnotobiotic animal models of human diseases. Cellular & Molecular Immunology, 8(2), 110-120. doi:10.1038/cmi.2010.67
- Jacob, C., Pastorino, A., Fahl, K., Carneiro-Sampaio, M., & Monteiro, R. (2008). Autoimmunity in IgA Deficiency: Revisiting the Role of IgA as a Silent Housekeeper. Journal Of Clinical Immunology, 28(S1), 56-61. doi:10.1007/s10875-007-9163-2
- Mu, Q., Kirby, J., Reilly, C., & Luo, X. (2017). Leaky Gut As a Danger Signal for Autoimmune Diseases. Frontiers In Immunology, 8. doi:10.3389/fimmu.2017.00598
- Fritscher-Ravens, A., Schuppan, D., Ellrichmann, M., Schoch, S., Röcken, C., & Brasch, J. et al. (2014). Confocal Endomicroscopy Shows Food-Associated Changes in the Intestinal Mucosa of Patients With Irritable Bowel Syndrome. Gastroenterology, 147(5), 1012-1020.e4. doi:10.1053/j.gastro.2014.07.046
- A, F. (2018). Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity, and cancer. – PubMed – NCBI. Ncbi.nlm.nih.gov. Retrieved from: https://journals.physiology.org/doi/full/10.1152/physrev.00003.2008
- Allergies | AAAAI. (2018). The American Academy of Allergy, Asthma & Immunology. Retrieved 19 July 2018, from https://www.aaaai.org/Conditions-Treatments/allergies
- Kamer, B., Wąsowicz, W., Pyziak, K., Kamer-Bartosińska, A., Gromadzińska, J., & Pasowska, R. (2012). Role of selenium and zinc in the pathogenesis of food allergy in infants and young children. Archives Of Medical Science, 6, 1083-1088. doi:10.5114/aoms.2012.32420
- Stier, H., & Bischoff, S. (2016). Influence of <em>Saccharomyces boulardii</em> CNCM I-745 on the gut-associated immune system. Clinical And Experimental Gastroenterology, Volume 9, 269-279. doi:10.2147/ceg.s111003 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5027949/
- Manzel, A., Muller, D., Hafler, D., Erdman, S., Linker, R., & Kleinewietfeld, M. (2013). Role of “Western Diet” in Inflammatory Autoimmune Diseases. Current Allergy And Asthma Reports, 14(1). doi:10.1007/s11882-013-0404-6
- Fabian, C., Kimler, B., & Hursting, S. (2015). Omega-3 fatty acids for breast cancer prevention and survivorship. Breast Cancer Research, 17(1). doi:10.1186/s13058-015-0571-6
- Scientific Opinion on the Tolerable Upper Intake Level of eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) and docosapentaenoic acid (DPA). (2012). EFSA Journal, 10(7). doi:10.2903/j.efsa.2012.2815
- Mark BJ, e. (2018). Are fish oil supplements safe in finned fish-allergic patients? – PubMed – NCBI . Ncbi.nlm.nih.gov. Retrieved 15 June 2018, from https://pubmed.ncbi.nlm.nih.gov/18926060/
- Walter, K., Corwin, E., Ulbrecht, J., Demers, L., Bennett, J., Whetzel, C., & Klein, L. (2012). Elevated thyroid stimulating hormone is associated with elevated cortisol in healthy young men and women. Thyroid Research, 5(1), 13. doi:10.1186/1756-6614-5-13 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3520819/
- Ranabir, S., & Reetu, K. (2011). Stress and hormones. Indian Journal Of Endocrinology And Metabolism, 15(1), 18. doi:10.4103/2230-8210.77573 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3079864/
- Dankers, W., Colin, E., van Hamburg, J., & Lubberts, E. (2017). Vitamin D in Autoimmunity: Molecular Mechanisms and Therapeutic Potential. Frontiers In Immunology, 7. doi:10.3389/fimmu.2016.00697 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5247472/
- Kim, D. (2017). The Role of Vitamin D in Thyroid Diseases. International Journal Of Molecular Sciences, 18(9), 1949. doi:10.3390/ijms18091949 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5618598/
- Prietl, B., Treiber, G., Pieber, T., & Amrein, K. (2013). Vitamin D and Immune Function. Nutrients, 5(7), 2502-2521. doi:10.3390/nu5072502 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3738984/
- How do I get the vitamin D my body needs?. (2018). Vitamin D Council. Retrieved 20 August 2018, from https://www.vitamindcouncil.org/about-vitamin-d/how-do-i-get-the-vitamin-d-my-body-needs/
- Janegova, A., Janega, P., Rychly, B., Kuracinova, K., & Babal, P. (2015). The role of Epstein-Barr virus infection in the development of autoimmune thyroid diseases . Endokrynologia Polska, 66(2), 132-136. doi:10.5603/ep.2015.0020 https://journals.viamedica.pl/endokrynologia_polska/article/view/EP.2015.0020/28584
- Wasserman EE, e. (2018). Infection and thyroid autoimmunity: A seroepidemiologic study of TPOaAb. – PubMed – NCBI . Ncbi.nlm.nih.gov. Retrieved 16 August 2018, from https://pubmed.ncbi.nlm.nih.gov/19811261/
- Choi, Y., Kim, T., Kim, E., Jang, E., Jeon, M., & Kim, W. et al. (2017). Association between thyroid autoimmunity and Helicobacter pylori infection. The Korean Journal Of Internal Medicine, 32(2), 309-313. doi:10.3904/kjim.2014.369 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5339455/#b20-kjim-2014-369
- Rowley, B., & Monestier, M. (2005). Mechanisms of heavy metal-induced autoimmunity. Molecular Immunology, 42(7), 833-838. doi:10.1016/j.molimm.2004.07.050 https://www.sciencedirect.com/science/article/abs/pii/S0161589004004146?via%3Dihub
- ATSDR – Public Health Statement: Total Petroleum Hydrocarbons (TPH). (1999). Atsdr.cdc.gov. Retrieved 14 August 2018, from https://www.atsdr.cdc.gov/phs/phs.asp?id=422&tid=75
- Abdel-Shafy, H., & Mansour, M. (2016). A review on polycyclic aromatic hydrocarbons: Source, environmental impact, effect on human health and remediation. Egyptian Journal Of Petroleum, 25(1), 107-123. doi:10.1016/j.ejpe.2015.03.011 https://www.sciencedirect.com/science/article/pii/S1110062114200237
- (2018). Epa.gov. Retrieved 14 August 2018, from https://www.epa.gov/sites/default/files/2014-03/documents/ffrrofactsheet_contaminant_perchlorate_january2014_final_0.pdf
- Learn about Polychlorinated Biphenyls (PCBs) | US EPA. (2015). US EPA. Retrieved 14 August 2018, from https://www.epa.gov/pcbs/learn-about-polychlorinated-biphenyls-pcbs
- Burek, C., & Talor, M. (2009). Environmental triggers of autoimmune thyroiditis. Journal Of Autoimmunity, 33(3-4), 183-189. doi:10.1016/j.jaut.2009.09.001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2790188/
- Allergic Reactions to Milk-Contaminated Nondairy Products | NEJM. (2018). New England Journal of Medicine. Retrieved 18 July 2018, from https://www.nejm.org/doi/full/10.1056/NEJM199104043241407
- Nutrient Uptake, Transport and Translocation in Cereals: Influences of Environment and Farming Conditions. (2018). Pub.epsilon.slu.se. Retrieved 12 July 2018, from https://pub.epsilon.slu.se/4083/1/malik_a_091030.pdf
- Balakireva, A., & Zamyatnin, A. (2016). Properties of Gluten Intolerance: Gluten Structure, Evolution, Pathogenicity and Detoxification Capabilities. Nutrients, 8(10), 644. doi:10.3390/nu8100644 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5084031/
- Haboubi, N., Taylor, S., & Jones, S. (2006). Coeliac disease and oats: a systematic review. Postgraduate Medical Journal, 82(972), 672-678. doi:10.1136/pgmj.2006.045443 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2653911/
- Simopoulos, A. (2002). The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomedicine & Pharmacotherapy, 56(8), 365-379. doi:10.1016/s0753-3322(02)00253-6 https://www.sciencedirect.com/science/article/abs/pii/S0753332202002536
- Fish and Omega-3 Fatty Acids. (2018). Heart.org. Retrieved 23 July 2018, from https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/fats/fish-and-omega-3-fatty-acids
- Patterson, E., Wall, R., Fitzgerald, G., Ross, R., & Stanton, C. (2012). Health Implications of High Dietary Omega-6 Polyunsaturated Fatty Acids. Journal Of Nutrition And Metabolism, 2012, 1-16. doi:10.1155/2012/539426
- Daley, C., Abbott, A., Doyle, P., Nader, G., & Larson, S. (2010). A review of fatty acid profiles and antioxidant content in grass-fed and grain-fed beef. Nutrition Journal, 9(1). doi:10.1186/1475-2891-9-10
- Omega-3 Poultry: The Science Inside the Food (2018). Otfarms.ca. Retrieved 19 July 2018, from https://www.otfarms.com/assets/food-flysheet-poultry.pdf (No longer available)
- Liu, R. (2013). Health-Promoting Components of Fruits and Vegetables in the Diet. Advances In Nutrition, 4(3), 384S-392S. doi:10.3945/an.112.003517 https://academic.oup.com/advances/article/4/3/384S/4591619
- Tsao, R. (2010). Chemistry and Biochemistry of Dietary Polyphenols. Nutrients, 2(12), 1231-1246. doi:10.3390/nu2121231
- Moskaug, J., Carlsen, H., Myhrstad, M., & Blomhoff, R. (2005). Polyphenols and glutathione synthesis regulation. The American Journal Of Clinical Nutrition, 81(1), 277S-283S. doi:10.1093/ajcn/81.1.277s https://academic.oup.com/ajcn/article/81/1/277S/4607567
- Lu, S. (2013). Glutathione synthesis. Biochimica Et Biophysica Acta (BBA) – General Subjects, 1830(5), 3143-3153. doi:10.1016/j.bbagen.2012.09.008
- Johnston, C., Meyer, C., & Srilakshmi, J. (1993). Vitamin C elevates red blood cell glutathione in healthy adults. The American Journal Of Clinical Nutrition, 58(1), 103-105. doi:10.1093/ajcn/58.1.103 https://academic.oup.com/ajcn/article-abstract/58/1/103/4715823?redirectedFrom=fulltext
- Kurutas, E. (2015). The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress: current state. Nutrition Journal, 15(1). doi:10.1186/s12937-016-0186-5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4960740/
- (2018). Ntp.niehs.nih.gov. Retrieved 25 July 2018, from https://ntp.niehs.nih.gov/ntp/htdocs/chem_background/exsumpdf/chaconinesolanine_508.pdf
- Konijeti, G., Kim, N., Lewis, J., Groven, S., Chandrasekaran, A., & Grandhe, S. et al. (2017). Efficacy of the Autoimmune Protocol Diet for Inflammatory Bowel Disease. Inflammatory Bowel Diseases, 23(11), 2054-2060. doi:10.1097/mib.0000000000001221
- Nishie, K., Gumbmann, M., & Keyl, A. (1971). Pharmacology of solanine. Toxicology And Applied Pharmacology, 19(1), 81-92. doi:10.1016/0041-008x(71)90192-x
- Perricone, C., De Carolis, C., & Perricone, R. (2009). Glutathione: A key player in autoimmunity. Autoimmunity Reviews, 8(8), 697-701. doi:10.1016/j.autrev.2009.02.020
https://www.sciencedirect.com/science/article/abs/pii/S1568997209000561 - (2018). Pdfs.semanticscholar.org. Retrieved 16 August 2018, from https://www.semanticscholar.org/paper/Oxidative-stress-and-nutritional-prevention-in-Sukkar-Rossi/38fba2e1b83ac7d1ca0b9af22ac2991505812d97
- Sears, M., & Genuis, S. (2012). Environmental Determinants of Chronic Disease and Medical Approaches: Recognition, Avoidance, Supportive Therapy, and Detoxification. Journal Of Environmental And Public Health, 2012, 1-15. doi:10.1155/2012/356798 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3270432/
- Dean P. Jones , Ralph J. Coates , Elaine W. Flagg , John W. Eley , Gladys Block , Raymond S. Greenberg , Elaine W. Gunter & Bethany Jackson (1992) Glutathione in foods listed in the national cancer institute’s health habits and history food frequency questionnaire, Nutrition and Cancer, 17:1, 57-75, DOI: 10.1080/01635589209514173https://www.researchgate.net/publication/21582175_Glutathione_in_Foods_Listed_in_the_National_Cancer_Institute’s_Health_Habits_and_History_Food_Frequency_Questionnaire
- Burek, C., & Talor, M. (2009). Environmental triggers of autoimmune thyroiditis. Journal Of Autoimmunity, 33(3-4), 183-189. doi:10.1016/j.jaut.2009.09.001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2790188/
[divider] [blog_posts style=”normal” type=”row” columns__md=”1″ depth_hover=”2″ ids=”105694,124838,142774,144284″ excerpt_length=”10″ image_height=”56.25%”]






2 comments on “Definitive Guide- How to Heal your Hashimoto’s Thyroiditis”
Bonnie Russell
This is so helpful. I would like to order a thyroid supplement. Which one do you recommend.
Dr. Michael Freedman
Hello Bonnie,
Thanks for reading the article. All supplement info is in the article. While we can’t give recommendations, if you have any specific questions about any of them, let me know!